 CFN – I had the opportunity to learn more about the new Telestroke program at CCH in Cornwall Ontario. Chief of Staff Dr. Lorne Scharf sat down and explained the program more in a one on one video interview. Dr. Scharf also gives more information about strokes and some of their symptoms.
CFN – I had the opportunity to learn more about the new Telestroke program at CCH in Cornwall Ontario. Chief of Staff Dr. Lorne Scharf sat down and explained the program more in a one on one video interview. Dr. Scharf also gives more information about strokes and some of their symptoms.
Dr. Scharf’s power point presentation on Telestroke. LINK More information on Telestroke. LINK
CCH Press Release
Cornwall Community Hospital (CCH) is proud to be designated as a licensed Telestroke site authorized by the Ontario Stroke Network (OSN). Telestroke is a two-way audiovisual linkup between a neurologist in a stroke centre and an emergency room physician. It is an approach to treating vascular strokes that allows a neurologist to provide remote treatment (from a tertiary site at a hospital in Ontario) for a stroke patient. The goal is for the neurologist to be able to talk to the patient and the physician about what symptoms they have experienced, evaluate the patient’s motor skills, view a computed tomography (CT) scan, make a diagnosis and prescribe treatment.
According to a 2011 study presented at the Canadian Stroke Congress, the use of long-distance video and data hookups to link remote community hospitals with stroke neurologists in large centres provides the same level of care as having everyone in the same room. This integral technology uses eHealth Ontario’s Emergency Neuro Image Transfer System (ENITS), a centralized web-based picture archiving and communication system for head scans that can be accessed and viewed by participating neurologists. “Telestroke makes it possible for a neurologist to be at the patient’s bedside, even when that patient is hundreds of miles away, and assist the local physician in determining the most effective therapy possible,” said Dr. Frank Silver, Neurologist and Medical Director, Telestroke.
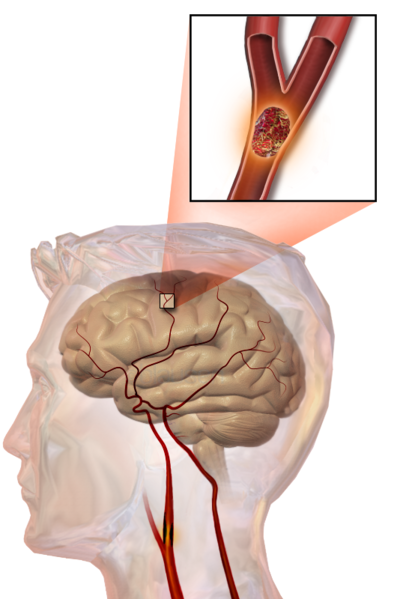
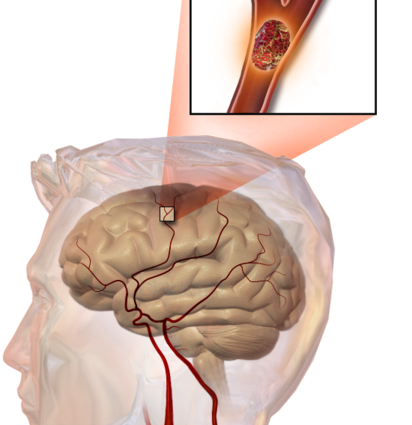
With an estimated 50,000 new reports each year, strokes are the third leading cause of death in Canada and are the leading cause of adult disability with 300,000 Canadians living with the aftereffects of an attack. A stroke is an emergency situation where time is of the essence. Early recognition of the five warning signs of a stroke or transient ischemic attack (TIA) may very well save a life if they are noticed and treated quickly enough. Sudden weakness, dizziness, trouble speaking or understanding, vision problems, and severe headaches are all symptoms of a potential stroke. If you notice yourself or someone else experiencing these symptoms do not hesitate to call 9-1-1 for immediate medical attention.
When a severe stroke is imminent, a drug known as a tissue plasminogen activator (tPA), a protein involved in breaking down blood clots, can be prescribed, and is most effective when administered within 4.5 hours of noticing symptoms. Over the past 12 months at CCH, 28 patients were assessed through Telestroke to determine if they should receive tPA. Of the 28 patients, 7 patients received the medication.
The best medicine for a stroke is still prevention. Studies show that up to 80 per cent of strokes can be prevented by working to reduce personal risk and modifying lifestyle activities such as: maintaining a healthy weight and diet, monitoring cholesterol and blood pressure, moderating alcohol use, abstaining from smoking, and exercising regularly.
As this program evolves it should be interesting to see besides how it impacts patients how it can help save our health system money.

this is excellent